At PMH, patients diagnosed with type 1 diabetes have traditionally stayed in hospital for 5 to 6 days while the families are educated on the different aspects of managing diabetes. It can be a very stressful time for families as they struggle to come to terms with the diagnosis and to take in vast amounts of information over a short period of time. It can also be very disruptive for families who are often juggling other children and work commitments.
We recently ran a study to compare the traditional model of care with a family-friendly, slower-paced, home-based alternative. Eligible patients were randomised to either usual care or to early discharge after basic practical education in diabetes management, approximately 48 hours after admission. Patients discharged early were visited by Hospital in the Home nurses to help with meal-time injections on the first two days and then a diabetes team made three home visits over two weeks to complete the education. The team include a diabetes nurse educator, accompanied by a dietician for two of the visits and a social worker for one. Patients had access to 24-hour phone support.
Fifty patients were included in the study, 25 in each group. All families completed patient satisfaction surveys at the end of the initial education. Three months after diagnosis families completed surveys on diabetes knowledge and the perceived impact of managing diabetes. Patients over 10 also completed a quality of life survey that measured impact, satisfaction and worries. These surveys were repeated nine months after diagnosis. Patients were followed up for 12 months at routine clinic visits.
More than two-thirds of families indicated that given the choice, they would prefer early discharge and home-based education for reasons including convenience, impact on the family and ability to take in information. There was no difference between the two groups in terms of diabetes knowledge, perceived impact of managing diabetes or self-reported quality of life measures in patients over 10, either at three or at nine months post-diagnosis.
There were no clinical differences between patients educated under the two different models during their first year following diagnosis. Blood sugar control and number of hospital readmissions and hypoglycaemic events were the same in both groups.
The study indicates that education for children newly diagnosed with type 1 diabetes can be safely delivered at home, allowing greater flexibility for families and giving them more time to adjust and learn about diabetes management. With adequate funding and additional staffing it may be possible to offer a similar model of care to other WA families in the future.
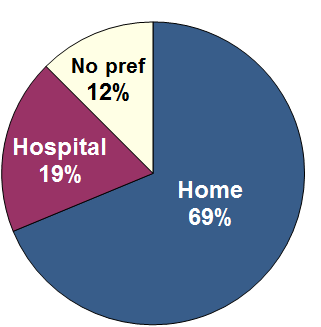
Results from Home education trial showed that most families preferred home education with no differences in the level of education or clinical outcomes in those educated at home or in hospital.
