Last month Diabetes WA and Princess Margaret Hospital held a family research event titled "Diabetes and Food - an update and research information evening." The evening included presentations from visiting key note speakers Dr Carmel Smart, Senior Paediatric Diabetes and Endocrine Dietitian, and Associate Professor Bruce King, Senior Paediatric Endocrinologist, both from John Hunter Children's Hospital in Newcastle.
The evening has stimulated discussion on both low carbohydrate diets (click here to see our previous article) and factors to consider when deciding on pre meal insulin doses. Current Type 1 Diabetes management guidelines recommend adjusting insulin doses for food based on the amount of carbohydrate eaten at each meal. This approach has been shown to reduce glucose variability through more accurate insulin dosing and allows for greater flexibility, which in turn has improved quality of life.
Carbohydrate counting is not limited to insulin pump therapy. Those on multiple daily injections, that is using a background basal insulin such as Lantus and giving rapid acting insulin prior to each meal, are also able to use insulin to carbohydrate ratios to determine pre meal insulin. Studies have shown that injection therapy using insulin to carbohydrate ratios can be just as effective as insulin pump therapy in reducing meal related glucose variability. Those on a twice daily insulin regimen also benefit from being aware of the carbohydrate content of their meals.
How accurately do you need to count carbohydrates?
Studies in children and adolescents with type 1 diabetes have demonstrated that insulin dosing for the actual carbohydrate content of a meal within 10g is effective for controlling blood glucose levels however an error of 20g is not effective.
Although current recommendations are to match insulin to carbohydrate content, many families report that meals high in fat and/or protein can cause high BGLs. This has been confirmed in recent studies and is clearly demonstrated in figure 1 which has come from a study undertaken here at PMH in collaboration with John Hunter Children's Hospital.
Figure 1 below represents the change in BGL (measured in mmol/L) following the 4 meals, all containing 30g of carbohydrate but varying amounts of protein and fat with '0' being the baseline, starting point
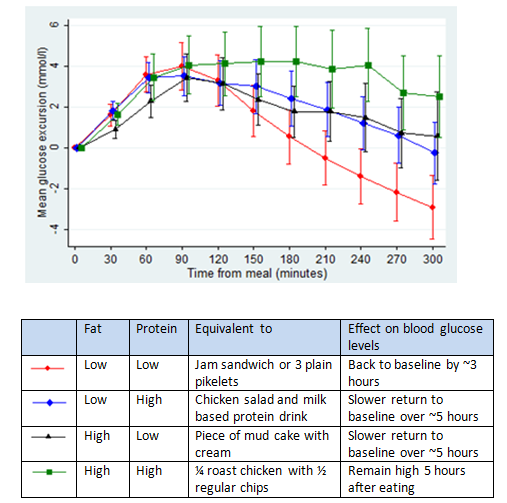
This suggests that there are instances when we may need to consider the timing and quantity of insulin for meals that are higher in fat and/or protein.
What can you do?
If you have noticed particular meals are causing high blood glucose excursions your clinical team is happy to look at individual strategies to help you manage.
In addition if you would like to look into carbohydrate counting or you have any other diet or nutrition related queries please contact the dietitians at PMH.
